NEUROLOGY
At AZ Integrated, our goal is provide a treatment plan that is entirely geared toward you. Our medical staff will spend time with you to understand your condition and recommend a treatment program that can help reduce or eliminate the source of the problem.
NEUROLOGY TEAM

Maninder Kahlon, MD
Dr Kahlon has been practicing in the Phoenix area for over 20 years, and brings a wealth of experience and knowledge to our practice. He is fellowship trained in Neurophysiology. He is on the board of Banner Health and has been associated with Arizona Integrated Physicians for years as both a member and board member. He has served on many committees in the years with the most recent Neuroscience Clinical Consensus Group through Banner Health Care Management. Dr Kahlon is a member of the American Medical Association, the American Academy of Neurology, and the American Association of Electrodiagnostic Medicine. Dr Kahlon is affiliated with Banner Boswell Medical Center, Banner Del Webb Medical Center, and Banner Thunderbird Medical Center. He is accepting new patients in our Phoenix, Sun City, and Sun City West locations.
Education
- 1989-1991 | Neurology Residency, Long Island Jewish Medical Center.
Albert Einstein College of Medicine, NY - 1991-1992 | Chief Resident, Neurology Department, Long Island Jewish Medical Center.
Albert Einstein College of Medicine, NY - 1992-1993 | Fellowship, Electrophysiology, Long Island Jewish Medical Center
Albert Einstein College of Medicine, NY
Interests:
Dr Kahlon is married to Ramit Kahlon, MD (Internal Medicine Physician) with two boys in college. He enjoys time with friends and family. He loves to play golf.

Swaraj Singh, MD
Dr. Singh’s areas of interest include vascular diseases affecting brain such as stroke, aneurysms, venous thrombosis etc, headaches and neurodegenerative disorders. He is member of American Academy of Neurology, American Heart Association, Society of Vascular and Interventional Neurology and American Medical Association. After graduating in 2002 from Govt. Medical College Patiala in India, Dr. Singh did a two year basic research fellowship in Experimental medicine at University of British Columbia, Canada where his research focused on neurodegenerative diseases such as Parkinson’s disease, ALS and Alzheimer’s disease.
Dr. Singh completed his neurology training at University of Arkansas for Medical Sciences and VA hospital, Little Rock AR, where he also served as chief resident. He did a fellowship in vascular neurology at University of Massachusetts. Dr. Singh has various publications during his training including co-authoring a textbook chapter. He has presented his research in various national and international conferences. He has been awarded many times including best resident of the year, Jeff Nicholas prize for dedication towards care of veterans and a prize for evidence based improvement in practice.
Did you know?
- Can Speak 4 languages
- Loves to play Indian classical Flute known as Bansuri.
- Married to a physician and has 2 lovely daughters.
For same day appointments please email appointments@azintegrated.com

Mona Mehta, MD
Dr. Mehta is a general neurologist, Board Certified by the American Board of Psychiatry and Neurology as well as board eligible for Clinical Neurophysiology, and she is a member of the American Academy of Neurology. She attended medical school at University of Missouri-Kansas City. She completed her internship, Neurology Residency, and Clinical Neurophysiology Fellowship at State University of New York Downstate. She has a special interest in neuromuscular disorders, but also practices general neurology.
For same day appointments please email appointments@azintegrated.com

Darry Johnson, MD
Dr. Darry Johnson is pleased to have joined Arizona Integrated Neurology as of March 2020. He is a board-certified neurologist who started his medical career here in Phoenix in August of 1996. He is now at the Glendale office near 63rd Avenue and Union Hills. He previously practiced in Peoria, Sun City, Sun City West, Scottsdale, and even did a stint in Flagstaff. He is excited to be in Glendale and looks forward to treating patients here.
Dr. Johnson is a general neurologist, but completed an extra fellowship in neurophysiology during his training years. As a result, he has added expertise in evaluating EEGs such as those done for seizure patients and in providing nerve conduction studies and EMGs for patients with possible carpal tunnel syndrome or other entrapment neuropathies, peripheral neuropathy, muscle disorders and weakness, to name a few.
He is also interested in taking care of patients with memory loss, dementia, and Alzheimer’s disease. He has expertise in Parkinson’s disease and other movement disorders such as essential tremor, restless leg syndrome, and similar conditions, some of which require deep brain stimulation (DBS) which he can adjust and manage. He is keenly interested in headache management, especially migraine diagnosis and treatment. He is adept at taking care of seizure disorders as well. He was the stroke director for 16 years at both Banner Boswell and Banner Del E. Webb Hospitals, and while he is now a purely outpatient neurologist, he holds stroke preventive practices near and dear to his heart, working closely with patients’ physicians and therapists after a stroke has occurred. He has been injecting Botox for over 25 years for such disease states as chronic migraine, stroke spasticity in arm or leg, blepharospasm, hemifacial spasm, and cervical dystonia.
He was recently named one of the prestigious Three Best Rated neurologists in Glendale, Arizona based on patient and peer reviews. Dr. Johnson’s philosophy remains simple: treat patients as if they were members of your own family. He believes clinical acumen and compassionate care can go hand in hand. Also, he takes listening to patients very seriously as he believes this is the core to excellent patient care.
Dr. Johnson earned his medical degree from the University of Kansas in 1991, finishing in the top 10% of his class. He then completed his internship at the University of Missouri in Kansas City and his neurology residency at the University of Arizona in Tucson, followed by a one year fellowship in neurophysiology at the same institution.
In his off hours, Dr. Johnson and the love of his life, Gina, enjoy the great outdoors. They are inseparable hiking partners and often get up early on weekends to enjoy the beautiful trails Arizona has to offer. Dr. Johnson and Gina are rabid Kansas City Chiefs fans and also root for the Kansas Jayhawks in college football and basketball. As far as baseball, they cheer for the Kansas City Royals and the Arizona Diamondbacks. They love God and their country.
Dr. Johnson is here for you! He is accepting new patients and will strive to be a neurologist you can depend on. If he cannot help you, he will do everything in his power to refer you to another physician who might. His office is at 6320 West Union Hills Drive, Building A, Suite 180 in Glendale, AZ, and he is there Monday through Friday. He looks forward to seeing you!

Puneet Dabas, MD
Dr. Puneet Dabas is a clinical neurologist with AZ integrated neuro and spine. Previously he was working in Prescott and Prescott valley, Arizona from 2017 till 2021. He completed his neurophysiology fellowship at MUSC with special interest in Epilepsy, Charleston SC from 2016-2017 after completing his residency (PGY4) at GRU Augusta GA from 2013-2016. Dr. Dabas completed his MD Physician degree from 1995-2001.
He is currently accepting new patients for consultation for all types of neurological disorders including stroke, dementia, multiple sclerosis, Parkinson’s disease, epilepsy, Essential tremors, headaches etc., as well as general neurological care.

Glen A. Halvorson MS, MD
Glen A. Halvorson M.S., M.D. has been performing EMGs since 1977. Board certified by the American Board of Electrodiagnostic Medicine since 1989, Dr. Halvorson is a former oral examiner for the EMG board, Qualified Medical Examiner for the State of California, Arizona State Physician Representative to the American Association of Electrodiagnostic and Neuromuscular Medicine for ten years, and a published author in the field.

Barry A. Hendin MD
Dr. Barry A. Hendin is a board certified neurologist with over 45 years of experience and a special clinical interest in Multiple Sclerosis. Originally from Missouri, Dr. Hendin received his medical degree from Washington University Medical School in 1968, interned at St. Louis Jewish Hospital from 1968-1969, and completed his residency and fellowship at Barnes Hospital in Missouri in 1972. He relocated to Arizona in the mid 1970s. An Air Force veteran, Dr. Hendin’s extensive career includes working as Chief of Neurology at Wright-Patterson AFB for two years and as Chief of Neurology for 35 years for Good Samaritan Hospital, as well as serving as Director of the Multiple Sclerosis Clinic at Banner University Medical Center from 2015 to 2020. He joined the Center for Neurology and Spine in 2020 as one of a core group of neurologists dedicated to the newly-launched, comprehensive and multidisciplinary Multiple Sclerosis Center of Arizona at the Center for Neurology and Spine.
Dr. Hendin is board certified by the American Board of Psychiatry and Neurology. He has been named a “Top Doc” every year (but one) between 1995 and 2019 and is the only neurologist to have received this honor more than 20 times. He was also named Health Professional of the Year by the National Multiple Sclerosis Society (NMSS), Arizona chapter, in 2007 and 2009. Dr. Hendin currently sits on the NMSS Board of Directors in addition to serving as the chief medical officer for the Multiple Sclerosis Association of America. With a passion for research and teaching as well as treating patients, he educates future doctors as a clinical professor of neurology at the University of Arizona Medical School and is involved in teaching locally, nationally, and internationally on topics related to MS. He stays apprised of the latest developments in MS diagnosis, treatment and management through his continuous involvement in research and emerging therapies, and has served as principal investigator for more than 115 clinical trials and counting.
Dr. Hendin’s clinical interest in Multiple Sclerosis began in 1993 when the very first disease-modifying medication for MS was developed. With science continually fueling new knowledge about the disease as well as a growing list of effective treatment options, Dr. Hendin feels his work with MS and MS patients fulfills his life’s mission: to live with purpose in a way that requires him to constantly learn and grow in the service of others. His philosophy is to take the best care he can of each individual patient, dealing comprehensively with the issues of MS from diagnosis through the course of the disease, with compassion and the overarching goal of delaying and reducing long-term disability. When he is not working, Dr. Hendin enjoys traveling and spending time with his wife, three grown children (including fellow Center for Neurology and Spine neurologist and MS expert Lori Hendin Travis), and his 16 grandchildren.
Education
MD– Washington University Medical School (St. Louis, Missouri)
Internship– St. Louis Jewish Hospital (St. Louis, Missouri)
Residency, Neurology– Barnes Hospital (St. Louis, Missouri)
Board Certification
American Board of Psychiatry and Neurology

Lori Travis MD
Dr. Lori Hendin Travis is a board certified neurologist with a clinical interest in Multiple Sclerosis. Dr. Travis earned her medical degree from the University of Arizona in 1998. She completed her internship at Good Samaritan Hospital, Phoenix in 1999 and her Neurology residency in 2002 at the Mayo Clinic, Minnesota, where she also served as Chief Resident. Dr. Travis has been an Assistant Professor of Clinical Neurology at the University of Arizona since 2004 and co-director of the Phoenix Neurological Associates Comprehensive Multiple Sclerosis Center. She joined the Center for Neurology and Spine in 2020 as one of a core group of neurologists dedicated to the newly-launched, comprehensive and multidisciplinary Multiple Sclerosis Center of Arizona at the Center for Neurology and Spine.
Dr. Travis is board certified by the American Board of Psychiatry and Neurology. She was named a Phoenix Magazine “Top Doc” in 2009, 2011, 2012 and 2016. She received the “Top Neurologist- Patient Reviews” award in 2015. She has authored and co-authored various poster presentations on MS, has appeared in several neurology publications, and has served as primary investigator and co-investigator on more than 20 clinical research trials, including a trial with a specific focus on Multiple Sclerosis and pregnancy.
As one of a minority of female specialists in her field, Dr. Travis sees herself as being in a unique position to reduce barriers when it comes to caring for the predominantly female MS patient population. Her care philosophy involves listening carefully to her patients’ needs and concerns, educating them about their options, advocating for them, and helping them be as healthy as possible. She enjoys the relational aspect of caring for patients with MS and encourages ongoing conversations based on her patients’ needs and the ongoing advancements in MS treatment that science has to offer. She thoroughly enjoys the teaching aspect of her work, both in the classroom and in the consultation room. When she’s not focused on multiple sclerosis alongside her father, fellow MS expert and Center for Neurology and Spine neurologist Dr. Barry A. Hendin, Dr. Travis enjoys spending time with her husband and eight children.
Education
MD– University of Arizona
Internship– Good Samaritan Hospital (Phoenix, Arizona)
Residency, Neurology– Mayo Clinic (Minnesota)
Board Certification
American Board of Psychiatry and Neurology

Vickram Kahlon, DO
Maninder Kahlon, MD
Swaraj Singh, MD
Mona Mehta, MD
Darry Johnson, MD
Puneet Dabas, MD
Glen A. Halvorson MS, MD
Vickram Kahlon, DO
Barry A. Hendin MD
Lori Travis MD
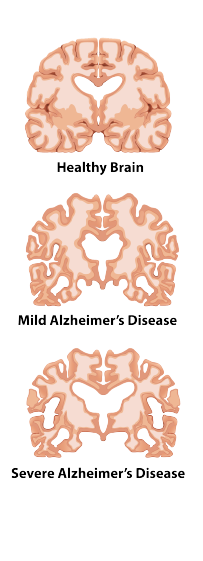
Alzheimer’s Disease
Alzheimer’s Disease (AD) accounts for 60% of cases of dementia. It is a chronic neurodegenerative disease that usually starts slowly and gets worse over time. The most common early symptom is difficulty in short-term memory loss. As the disease advances, symptoms can include: language issues, disorientation, mood swings, loss of motivation, not managing ADL’s, and behavior issues. As a person’s condition declines, they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the average life expectancy following diagnosis is three to nine years.
The cause of Alzheimer’s disease is poorly understood. About 70% of the risk is believed to be genetic with many genes usually involved. Other risk factors include: a history of head injuries, depression or hypertension. The disease process is associated with plaques and tangles in the brain. A probable diagnosis is based on the history of the illness and cognitive testing with medical imaging and blood tests to rule out other possible causes. Initial symptoms are often mistaken for normal aging. Examination of brain tissue is needed for a definite diagnosis. Mental and physical exercise, and avoiding obesity may decrease the risk of AD. There are no medications or supplements with evidence to support their use.
No treatments stop or reverse its progression, though some may temporarily improve symptoms. Affected people increasingly rely on others for assistance, often placing a burden on the caregiver; the pressures can include social, psychological, physical, and economic elements. Exercise programs are beneficial with respect to activities of daily living and potentially improve outcomes. Treatment of behavioral problems or psychosis due to dementia with antipsychotics is common but not usually recommended due to there often being little benefit and an increased risk of early death.
Multiple Sclerosis
Multiple Sclerosis (MS) is a chronic, often disabling disease that attacks the central
nervous system (AZ Integrated), which is made up of the brain, spinal cord, and optic nerves.
Symptoms may be mild, such as numbness in the limbs, or severe, such as paralysis
or loss of vision. The progress, severity, and specific symptoms of MS are
unpredictable and vary from one person to another. Today, new treatments and
advances in research are giving new hope to people affected by the disease.
Symptoms can include:
• Paralysis
• Numbness
• Balance Impairment
• Visual Loss
• Dizziness
• And Other Symptoms.
The disease is likely the result of a genetic predisposition, and some environmental
trigger that causes one’s own immune system to attack the brain, spinal cord, and
optic nerves. The diagnosis and treatment of Multiple Sclerosis can be difficult and is
best handled by an experienced Neurologist.
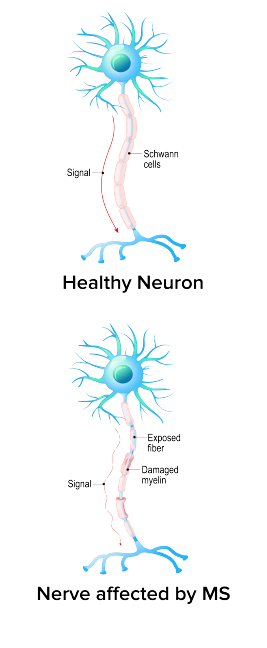
MULTIPLE SCLEROSIS IS THOUGHT TO BE AN AUTOIMMUNE DISEASE
The body’s own defense system attacks myelin, the fatty substance that surrounds
and protects the nerve fibers in the central nervous system. The nerve fibers
themselves can also be damaged. The damaged myelin forms scar tissue (sclerosis),
which gives the disease its name. When any part of the myelin sheath or nerve fiber
is damaged or destroyed, nerve impulses traveling to and from the brain and spinal
cord are distorted or interrupted, producing the variety of symptoms that can occur.
Most people with MS learn to cope with the disease and continue to lead satisfying,
productive lives.
FOUR COURSES OF MULTIPLE SCLEROSIS
People with Multiple Sclerosis can typically experience one of four disease courses,
each of which might be mild, moderate, or severe.
Relapsing-Remitting Multiple Sclerosis
People with this type of MS experience clearly defined attacks of worsening
neurologic function. These attacks—which are called relapses, flare-ups, or
exacerbations —are followed by partial or complete recovery periods (remissions),
during which no disease progression occurs. Approximately 85% of people are
initially diagnosed with relapsing-remitting MS.
Primary-Progressive Multiple Sclerosis
This disease course is characterized by slowly worsening neurologic function from
the beginning—with no distinct relapses or remissions. The rate of progression may
vary over time, with occasional plateaus and temporary minor improvements.
Approximately 10% of people are diagnosed with primary-progressive MS.
Secondary-Progressive Multiple Sclerosis
Following an initial period of relapsing-remitting MS, many people develop a
secondary-progressive disease course in which the disease worsens more steadily,
with or without occasional flare-ups, minor recoveries (remissions), or plateaus.
Before the disease-modifying medications became available, approximately 50% of
people with relapsing-remitting MS developed this form of the disease within 10
years. Long-term data are not yet available to determine if treatment significantly
delays this transition.
Progressive-Relapsing Multiple Sclerosis
In this relatively rare course of MS (5%), people experience steadily worsening
disease from the beginning, but with clear attacks of worsening neurologic function
along the way. They may or may not experience some recovery following these
relapses, but the disease continues to progress without remissions.
Since no two people have exactly the same experience of MS, the disease course
may look very different from one person to another. And, it may not always be clear
to the physician—at least right away—which course a person is experiencing.
For more important information about Multiple Sclerosis, check out Just the Facts.
SOME IMPORTANT FACTS
MS is a chronic, unpredictable neurological disease that affects the central nervous
system.
Different people are likely to experience very different symptoms.
MS is different from muscular dystrophy (MD), which is a group of disorders that
cause progressive and irreversible wasting away of muscle tissue. Although MD has
some symptoms in common with MS—such as weakness and problems with walking
—MD affects the muscles directly while MS affects the central nervous system.
MS is not contagious and is not directly inherited.
Most people with MS have a normal or near-normal life expectancy.
The majority of people with MS do not become severely disabled.
There are now FDA-approved medications that have been shown to reduce the
number of relapses and “modify” or slow down the underlying course of MS.
People who are diagnosed with a Clinically Isolated Syndrome (CIS) have had one
episode of neurologic damage that is similar to the damage that occurs in MS, but
they have not yet met the criteria for a definite diagnosis of MS.
IS THERE CURRENTLY A CURE?
There is no known cure for Multiple Sclerosis, however, there are treatments that are
effective in reducing the likelihood of worsening of the disease, and, there are a
multitude of new treatments in current research and development that will soon be
available.
For more information on Multiple Sclerosis, or to speak with one of our physicians
regarding treatment options, please contact us to schedule an appointment.
Cervical Dystonia
Cervical Dystonia is a movement disorder characterized by involuntary contractions
of neck muscles those results in neck pain, and involuntary head position. Patients
complain that they cannot keep their head in a normal position. It may pull to the side, twist, or veer to an abnormal position. Some people refer to this as “torticollis”.
Medications may be ineffective in many patients. Botox is the most effective treatment for this illness, and may offer three months or more of relief. Treatments
generally have to be done in three or four month intervals to assure continued benefit. The injections are minimally uncomfortable, and are done in our clinic.
Seizures
Seizures are generally described in two major groups of seizures, primary
generalized seizures and partial seizures. The difference between these types is in
how and where they begin. A new way of naming seizures has been developed by
epilepsy specialists, but most often these common names are still used.
Primary generalized seizures begin with a widespread electrical discharge that
involves both sides of the brain at once. Hereditary factors are important in many of
these seizures.
Partial seizures begin with an electrical discharge in one limited area of the brain.
Many different things can cause partial seizures, for example head injury, brain
infection, stroke, tumor, or changes in the way an area of the brain was formed
before birth called cortical dysplasias. Many times, no known cause is found, but
genetic factors may be important in some partial seizures.
Partial seizures can be broken down further, depending on whether a person’s
awareness or consciousness (the ability to respond and remember) is affected.
There are six types of generalized seizures. The most common is the generalized
convulsion, also called the grand-mal seizure or a tonic-clonic seizure. The patient
loses consciousness and usually collapses. The loss of consciousness is followed by
generalized body stiffening ,tonic, for 30 to 60 seconds, then by violent jerking,
clonic for 30 to 60 seconds, after which the patient goes into the postictal phase.
During tonic-clonic seizures, injuries and accidents may occur, such as tongue biting
and urinary incontinence.
Absence seizures cause a short loss of consciousness lasting only a few seconds
with few or no symptoms. The patient, most often a child, typically interrupts an
activity and stares blankly. These seizures begin and end abruptly and may occur
several times a day. Patients are usually not aware that they are having a seizure,
except that they may be aware of “losing time.”
Myoclonic seizures consist of sporadic jerks, usually on both sides of the body.
Patients sometimes describe the jerks as brief electrical shocks. When violent, these
seizures may result in dropping or involuntarily throwing objects.
Clonic seizures are repetitive, rhythmic jerks that involve both sides of the body at
the same time.
Tonic seizures are characterized by stiffening of the muscles.
Atonic seizures consist of a sudden and general loss of muscle tone, particularly in
the arms and legs, which often results in a fall.
The type of treatment prescribed will depend on several factors, including the
frequency and severity of the seizures and the person’s age, overall health, and
medical history.

Headaches & Migraines
A headache or cephalgia is pain of the head or neck. Headaches can result from a
wide range of causes both benign and more serious. Brain tissue itself is not
sensitive to pain as it lacks pain receptors. Rather, the pain is caused by disturbance
of the pain-sensitive structures around the brain. Nine areas of the head and neck
have these pain-sensitive structures, which are the cranium, muscles, nerves,
arteries and veins, subcutaneous tissues, eyes, ears, sinuses and mucous
membranes. There are a number of different classification systems for headaches.
The most well-recognized is that of the International Headache Society. Headache is
a non-specific symptom, which means that it has many possible causes, including
fatigue and sleep deprivation, stress, the effects of medications and recreational
drugs, viral infections and common colds, head injury, rapid ingestion of a very cold
food or beverage, dental or sinus issues, and many more.
A migraine headache can cause intense throbbing or a pulsing sensation in one area
of the head and is commonly accompanied by nausea, vomiting, and extreme
sensitivity to light and sound.
Migraine attacks can cause significant pain for hours to days and be so severe that
all you can think about is finding a dark, quiet place to lie down. Some migraines are
preceded or accompanied by sensory warning symptoms (aura), such as flashes of
light, blind spots, or tingling in your arm or leg. Medications can help reduce the
frequency and severity of migraines. If treatment hasn’t worked for you in the past,
talk to your doctor about trying a different migraine headache medication. The right
medicines, combined with self-help remedies and lifestyle changes, may make a big
difference.


